-
- 1800 2010
- EN

News
Array
(
[0] => stdClass Object
(
[id] => 1167
[id_crawler] =>
[category_product] => NULL
[thumbnail] => dsc05415.jpg
[album] =>
[url_video] =>
[is_status] => 1
[is_featured] => 0
[is_form] => 0
[displayed_time] => 2023-12-26
[program] => 0
[number] => 1
[viewed] => 0
[type] =>
[type_career] =>
[level] =>
[address] =>
[address_career] =>
[expiration_time] => 0000-00-00
[created_time] => 2023-12-26 08:49:01
[updated_time] => 2024-09-04 09:29:49
[files] =>
[salary] =>
[time] =>
[created_by] => 63
[is_table_content] => 1
[language_code] => en
[slug] => Gentis-sponsored-and-presented-at-the-assisted-reproductive-technology-ART-symposium-titlted-a-christmas-gift-a-happy-begining
[title] => GENTIS sponsored and presented at the assisted reproductive technology (ART) symposium titled "A Christmas Gift - A Happy Beginning”.
[description] => The 2023 "A Christmas Gift - A Happy Beginning" Assisted Reproductive Technology (ART) Symposium at Hai Phong International Women's and Children's Hospital officially concluded successfully with the participation of over 100 infertile couples. GENTIS is honored to have been the event’s Diamond Sponsor and presented a scientific paper titled "Karyotype: Applications and Result Interpretation in Assisted Reproduction."
[content] => “A Christmas Gift - A Happy Beginning” is a special event organized exclusively for infertile couples. This occasion served as an opportunity for clients to be updated with insights into assisted reproductive technology (ART) and win exciting prizes to support their journey to parenthood in 2024.
 The "A Christmas Gift - A Happy Beginning" symposium was a resounding success.
The "A Christmas Gift - A Happy Beginning" symposium was a resounding success.
In his opening remarks, Specialist level 1 Nguyen Duc Thuan, MD. (Director of Assisted Reproductive Center at Hai Phong International Women's and Children's Hospital) expressed his understanding of the challenges faced by infertile couples: “Within 10 years of experience in the field of medicine, Dr. Thuan and his team deeply understand the hopes and feelings of couples struggling with infertility. The procedure of treating infertility is a complex journey that requires serious time, effort, and can be emotionally, physically, and financially taxing. Noticing that not all couples have ample time to thoroughly investigate treatment for infertility, HP Fertility organized this symposium.”
At the event, parents listened to Dang Truong Son, MSc. (Head of the IVF HP Fertility Laboratory), Diep Minh Quang, MSc.MD. (IVF FP Fertility) and Nguyen Thi Huyen, MSc.MD. (GENTIS R&D Consultant) sharing proficient knowledge within the field of assisted reproduction. Following the speech, couples acquired knowledge of common causes of infertility and general challenges. Besides, they were introduced to contemporary assisted reproductive techniques that are currently in use.
In addition, experts also provided updates on the latest trends to increase treatment success rates. Moreover, participants also got the chance to get individual advice and consultations with top fertility experts. As an added benefit, participants were eligible for exclusive offers and appealing prizes worth up to 400 million VND.
 Nguyen Thi Huyen, MSc.MD. (GENTIS R&D Consultant) presented the report with the subject “Karyotype: Applications and Result Interpretation in Assisted Reproduction."
Nguyen Thi Huyen, MSc.MD. (GENTIS R&D Consultant) presented the report with the subject “Karyotype: Applications and Result Interpretation in Assisted Reproduction."
The presentation delivered by Ms. Nguyen Thi Huyen, MSc.MD., R&D Consultant at GENTIS, on "Karyotype: Applications and Genetic Counseling in Assisted Reproduction" gained remarkable interest from parents. A karyotype test, according to Ms. Huyen, is a diagnostic workup performed to identify whether a fetus has chromosomal abnormalities linked to genetic disorders. Karyotype testing can be carried out at different stages of pregnancy, including pre-conception, prenatal, and postnatal periods.
Karyotype testing is most commonly used in prenatal care, helping to identify chromosomal conditions that may influence a developing baby. In assisted reproduction, karyotype testing is essential to diagnose genetic causes of infertility, miscarriage, and birth defects, and provide following treatment plans.
For couples with chromosomal abnormalities, there is an increased risk of transmitting these mutations to the fetus, leading to adverse outcomes. Preimplantation genetic testing for aneuploidy (PGT-A) can be a viable option to mitigate these dangers. It is fundamental to experience genetic counseling before and after karyotype testing. Currently, GENTIS offers karyotype testing on three types of samples: peripheral blood, amniotic fluid, and umbilical cord blood.
With the capacity to perform tens of thousands of tests annually and laboratories systems accredited to ISO 9001:2015 and ISO 15189:2012 standards, GENTIS is committed to developing tailor-made genetic technologies to the needs of Vietnamese patients, providing significant benefit in the diagnosis and treatment of diseases, as well as assisted reproduction. GENTIS continues to solidify its leading position in the field of genetic testing, earning the trust of our partners and customers.
 GENTIS was honored to be the Diamond Sponsor of the "A Christmas Gift - A Happy Beginning” symposium.
GENTIS was honored to be the Diamond Sponsor of the "A Christmas Gift - A Happy Beginning” symposium.
Additionally, GENTIS impressed participants with our exhibition booth showcasing advanced diagnostic tests. At the booth, parents were able to learn more about GENTIS's comprehensive range of maternal and neonatal screening tests, including Non-Invasive Prenatal Testing (NIPT) and newborn screening. We extend our congratulations on the successful symposium.
[content_more] =>
[meta_title] => GENTIS sponsored and presented at the assisted reproductive technology (ART) symposium
[meta_description] => GENTIS is honored to have been the event’s Diamond Sponsor and presented a scientific paper titled "Karyotype: Applications and Result Interpretation in Assisted Reproduction."
[meta_keyword] => Gentis
[thumbnail_alt] =>
[post_id] => 1167
[category_id] => 4
)
[1] => stdClass Object
(
[id] => 1166
[id_crawler] =>
[category_product] => NULL
[thumbnail] => web.jpg
[album] =>
[url_video] =>
[is_status] => 1
[is_featured] => 0
[is_form] => 0
[displayed_time] => 2023-12-22
[program] => 0
[number] => 1
[viewed] => 0
[type] =>
[type_career] =>
[level] =>
[address] =>
[address_career] =>
[expiration_time] => 0000-00-00
[created_time] => 2023-12-22 08:56:55
[updated_time] => 2024-09-04 09:25:25
[files] =>
[salary] =>
[time] =>
[created_by] => 63
[is_table_content] => 1
[language_code] => en
[slug] => Gentis-partnered-with-the-program-Gifts-gleaming-christmas-cheer-at-thanh-nhan-hospital
[title] => GENTIS partnered with the program “Gifts gleaming - Christmas cheer” at Thanh Nhan Hospital
[description] => From December 22nd, 2023 to January 22nd, 2024, GENTIS collaborated with Department 2 of Obstetrics and Gynecology - Thanh Nhan Hospital to conduct the program “Gifts gleaming - Christmas cheer”. This program exclusively targeted pregnant mothers when registering for pregnancy consulting and newborn screening at Department 2 of Obstetrics and Gynecology of Thanh Nhan Hospital. GENTIS is honored to be the main sponsor of this program.
[content] => Currently, there has been a significant increase in congenital anomalies in newborns. These conditions can emerge from various factors, including environmental pollution, dietary exposure to chemicals, maternal psychological stress, and genetic predisposition. According to the data of the Ministry of Health, it is estimated that around 1.5 million babies are born each year in Vietnam, with 2-3% of them affected by genetic disorders or congenital mutations including Down syndrome, neural tube defects, and thalassemia.
Thus, newborn screening is considered the most proficient method for early detection of these birth defects. This screening test allows doctors to identify infants at risk for genetic disorders or congenital anomalies, facilitating timely diagnosis and intervention.
Early detection and treatment can not only significantly assist in the child’s normal development, but also diminish the burden on families and society due to the fact that these congenital anomalies or underlying diseases can essentially affect a newborn's physical, mental, and cognitive development, and can even be fatal.

Understanding the significance of newborn screening tests, GENTIS is honored to partner with the Department 2 of Obstetrics and Gynecology - Thanh Nhan Hospital in organizing the event “Gifts gleaming - Christmas cheer”. As a special gift, GENTIS will present an adorable teddy bear and a special product to clients who register for pregnancy consulting and newborn screening at the Department 2 of Obstetrics and Gynecology, Thanh Nhan Hospital. This gift bundle acts as a small token from GENTIS and the hospital to empower families to become more aware of and interested in this service.
As of now, GENTIS is providing an assortment of newborn screening test packages for parents to choose. A distinctive feature of GENTIS's newborn screening packages is the utilization of specialized techniques to identify newborns at risk of having congenital anomalies and disorders related to endocrine, metabolic, and genetic abnormalities that may not present clinically during the neonatal period. GENTIS is committed to continuous improvement to ensure the accuracy and precision of every procedure and result, fulfilling our mission of enhancing the physical and intellectual well-being of the Vietnamese people.
[content_more] =>
[meta_title] => GENTIS partnered with the program “Gifts gleaming - Christmas cheer” at Thanh Nhan Hospital
[meta_description] => From December 22nd, 2023 to January 22nd, 2024, GENTIS collaborated with Department 2 of Obstetrics and Gynecology - Thanh Nhan Hospital to conduct the program “Gifts gleaming - Christmas cheer”
[meta_keyword] => Gentis
[thumbnail_alt] =>
[post_id] => 1166
[category_id] => 4
)
[2] => stdClass Object
(
[id] => 1165
[id_crawler] =>
[category_product] => NULL
[thumbnail] => hasam_2023/gentis-322.jpg
[album] =>
[url_video] =>
[is_status] => 1
[is_featured] => 0
[is_form] => 0
[displayed_time] => 2023-12-13
[program] => 0
[number] => 1
[viewed] => 0
[type] =>
[type_career] =>
[level] =>
[address] =>
[address_career] =>
[expiration_time] => 0000-00-00
[created_time] => 2023-12-13 13:42:00
[updated_time] => 2024-09-04 11:06:09
[files] =>
[salary] =>
[time] =>
[created_by] => 63
[is_table_content] => 0
[language_code] => en
[slug] => Gentis-sponsored-and-reported-at-the-HASAM-2023-Annual-Scientific-conference
[title] => GENTIS sponsored and reported at the HASAM 2023 Annual Scientific Conference
[description] => On December 10, 2023, the Hanoi Society of Assisted Reproduction held the HASAM 2023 Annual Scientific Conference at the Daewoo Hotel in Hanoi. GENTIS was honored to be a Gold Sponsor and presented a scientific report on the topic: "Personalized Treatment of Infertility Based on Gene and Genetic Testing: Current Status and Trends."
[content] => The HASAM 2023 Annual Scientific Conference attracted the attendance of over 300 delegates, including embryology experts, lab directors, clinical doctors, heads of leading Assisted Reproduction centers nationwide, and international assisted reproduction experts. This event provided a platform for delegates to connect, exchange knowledge, learn, and stay updated on clinical and practical aspects of assisted reproduction, including: ovarian stimulation, embryo transfer, infertility treatment based on genetic testing, male infertility solutions, ect.
The main theme of this year's conference was "Updating Outstanding Achievements to Enhance Success Rates in Assisted Reproduction," featuring 26 high-quality scientific reports. A highlight of the conference was the genetics session, co-chaired by Le Thi Lan Phuong, M.Sc., M.D. (Vinmec Hospital) and Pham Dinh Minh, Ph.D. (Director of GENTIS R&D), which included four presentations focusing on embryos, genetics, PGT techniques, andrology testing, etc.
 The HASAM 2023 Annual Scientific Conference took place on December 10, 2023.
The HASAM 2023 Annual Scientific Conference took place on December 10, 2023.
During the discussion session, the report titled "Sexually Transmitted Diseases and Infertility: Clinical Significance of Testing and Treatment Approaches" by Nguyen Ba Hung, M.Sc., M.D. (Vinmec Hospital) garnered significant attention from attendees. According to Doctor Hung, he highlighted that sexually transmitted diseases (STDs) are complex conditions impacting all stages of male and female reproduction (eggs, sperm, embryos, babies,...). Currently, PCR testing for 12 pathogens is the most prevalent NAAT method for detecting and quantifying STI agents. It is considered the gold standard for clinical diagnosis, boasting a sensitivity and specificity exceeding 98%, and can be performed simultaneously for multiple pathogens.
In his presentation, Doctor Hung also included information about GENTIS's STDs combo test for 12 pathogens, utilizing Realtime PCR technology (Caregene). He expressed high praise for GENTIS's STDs testing, recognizing its ability to optimize diagnosis accuracy for doctors and the costs for patients.
 Nguyen Ba Hung, M.Sc., M.D. (Vinmec Hospital) presented a report entitled "Sexually Transmitted Diseases and Infertility: Clinical Significance of Testing and Treatment Approaches."
Nguyen Ba Hung, M.Sc., M.D. (Vinmec Hospital) presented a report entitled "Sexually Transmitted Diseases and Infertility: Clinical Significance of Testing and Treatment Approaches."
A highly debated topic at the conference was the report presented by Specialist level 1 Doctor Nguyen Thanh Trung (Hanoi Hospital of Infertility and Andrology) titled "Clinical Outcomes of Mosaic Embryo Transfers at Hanoi Hospital of Infertility and Andrology." This research, which is part of a collaborative scientific project between the hospital and GENTIS, aimed to assess the clinical outcomes of mosaic embryo transfers, specifically focusing on implantation rates, miscarriage rates, and live birth rates. Doctor Trung, who was directly involved in the project, provided valuable insights for clinicians, suggesting that mosaic embryos with less than 50% mosaicism could be considered for patients lacking euploid embryos. He also emphasized the crucial need for thorough risk assessment and comprehensive counseling for patients undergoing mosaic embryo transfer.
 Specialist level 1 Doctor Nguyen Thanh Trung (Hanoi Infertility and Andrology Hospital) presented research titled "Clinical Outcomes of Mosaic Embryo Transfers at Hanoi Hospital of Infertility and Andrology."
Specialist level 1 Doctor Nguyen Thanh Trung (Hanoi Infertility and Andrology Hospital) presented research titled "Clinical Outcomes of Mosaic Embryo Transfers at Hanoi Hospital of Infertility and Andrology."
Especially, GENTIS was particularly proud that Pham Dinh Minh, Ph.D. (Director of GENTIS R&D Center) was invited to chair and present a report titled "Personalized Treatment of Infertility Based on Gene and Genetic Testing: Current Status and Trends." He considered that gene/genetic testing was becoming prevalent in assisted reproduction and obstetrics in Vietnam. In the future, gene/genetic testing will become more personalized to individual patients, aiding in treatment and proactive healthcare management.
Besides, Dr. Minh also shared insights into GENTIS's testing ecosystem for screening, diagnosis, and personalized treatment in assisted reproduction, including:
- Testing for Parents and Embryos:
- Mother: HPV, Thalassemia, Thrombophilia, Advanced Genetic Screening...
- Father: Andrology testing kit, Karyotype; Advanced Genetic Screening for 150 genes...
- Embryo: PGT-A/SR, PGT-M, PGT-One, PGT-Plus, ASEM Test
- Embryo Transfer Environment Testing:
- Genratest: Personalized embryo transfer timing
- PMTest: Uterine lining microbiome identification
- Maternal and Fetal Health Testing:
Preeclampsia, Antiphospholipid syndrome, NIPT-basic/Geneva, Newborn Screening
 Pham Dinh Minh, Ph.D. (Director of GENTIS R&D Center) presented a report titled "Personalized Treatment of Infertility Based on Gene and Genetic Testing: Current Status and Trends."
Pham Dinh Minh, Ph.D. (Director of GENTIS R&D Center) presented a report titled "Personalized Treatment of Infertility Based on Gene and Genetic Testing: Current Status and Trends."
Proudly partnering as a Gold Sponsor of the HASAM 2023 Annual Scientific Conference, GENTIS impressed attendees with its product showcase booth and engaging activities. Many conference participants checked in at the booth to receive a complimentary copy of the book "Male Infertility Through the Lens of Genetics." The event also featured a mini-game with numerous gifts as a token of appreciation for the esteemed doctors in the Conference.
 The GENTIS product exhibition booth drew significant attention from numerous attendees with its many engaging activities.
The GENTIS product exhibition booth drew significant attention from numerous attendees with its many engaging activities.
These were some of the highlights of GENTIS's participation in the HASAM 2023 Annual Scientific Conference. Through this year's conference, GENTIS hoped to bring its comprehensive gene testing ecosystem closer to doctors, experts, and healthcare professionals in Vietnam. Congratulations once again on the resounding success of the conference.
[content_more] => [meta_title] => GENTIS sponsored and reported at the HASAM 2023 Annual Scientific Conference [meta_description] => On December 10, 2023, the Hanoi Society of Assisted Reproduction held the HASAM 2023 Annual Scientific Conference at the Daewoo Hotel in Hanoi [meta_keyword] => AssistedReproducted,Gentis,HASAM2023,Conference,Symposium [thumbnail_alt] => [post_id] => 1165 [category_id] => 4 ) [3] => stdClass Object ( [id] => 1164 [id_crawler] => [category_product] => NULL [thumbnail] => hasam_2023/trước-hỘi-nghị-hasam.jpg [album] => [url_video] => [is_status] => 1 [is_featured] => 0 [is_form] => 0 [displayed_time] => 2023-12-06 [program] => 0 [number] => 1 [viewed] => 0 [type] => [type_career] => [level] => [address] => [address_career] => [expiration_time] => 0000-00-00 [created_time] => 2023-12-06 09:47:51 [updated_time] => 2024-08-19 16:16:54 [files] => [salary] => [time] => [created_by] => 63 [is_table_content] => 0 [language_code] => en [slug] => gentis-gold-sponsor-of-the-hasam-2023-annual-scientific-conference [title] => GENTIS - Gold Sponsor of the HASAM 2023 Annual Scientific Conference [description] => The HASAM 2023 Annual Scientific Conference, organized by the Hanoi Society of Assisted Reproduction, will take place on December 10, 2023, at the Daewoo Hotel, Hanoi. GENTIS is honored to be the Gold Sponsor of this year’s conference. [content] =>
After 45 years of development worldwide and 25 years in Vietnam, the field of Assisted Reproductive Technology (ART) has increasingly played a crucial role and achieved significant success in helping infertile couples realize their dreams of becoming parents. Vietnam is among the countries with rapid development in both the quantity and quality of infertility management.
However, despite many remarkable scientific advancements, the success rate for many couples has not yet met expectations. To improve treatment quality, the Hanoi Society of Assisted Reproduction is organizing its 4th annual scientific conference to update knowledge, share scientific and technical advancements, and exchange experiences in in-vitro fertilization (IVF) with specialists and doctors from both Vietnam and abroad.
This special and engaging conference will feature high-quality presentations from experienced domestic and international experts. Attendees will include the Executive Committee of the Hanoi Society of Assisted Reproduction, embryology experts, lab directors, clinical doctors, leaders of leading ART centers in Vietnam, and international ART experts.

At the 2023 conference, GENTIS is honored to be the GOLD sponsor and will present various exciting programs:
- A modern booth showcasing the full ecosystem of testing services.
- A program introducing and offering FREE copies of the book "Male Infertility through the Lens of Genetics."
- A mini-game with gifts and other appreciation tokens for our esteemed doctors.
In particular, GENTIS representative Dr. Pham Dinh Minh will present a report titled: "Personalized Treatment of Infertility Based on Genetic and Genomic Testing: Current Status and Trends."
We warmly invite our esteemed doctors to follow the Conference Agenda:


The main theme of the symposium was "New challenges in obstetrics and gynecology and current practice perspectives". Through 4 seminar sessions, with 98 high-quality scientific reports, nearly 600 participants had the opportunity to update practical and in-depth knowledge on a number of topics such as: Prenatal pathology - Fetal medicine; New perspectives in Obstetrics and Gynecology, infertility; Advances in assisted reproductive techniques... Speakers are experienced leading experts in the field of obstetrics in Vietnam.
 The 10th Central region and Central Highlands Obstetrics and Gynecology Conference was held on April, 24th and 25th 2023
The 10th Central region and Central Highlands Obstetrics and Gynecology Conference was held on April, 24th and 25th 2023
In the second session of the conference, Nguyen Canh Chuong, MSc. MD. (Director of the Training and Steering Center of Hanoi Hospital of Obstetrics and Gynecology) presented the report: "Expanded NIPT: From a clinical perspective".
Dr. Chuong said that the expanded NIPT test will screen for more recessive genetic diseases with a combined frequency of 1/600 of acquired diseases, equivalent to the incidence of Down syndrome. Although the expanded NIPT has not been officially recommended by medical associations due to the lack of data evidence, according to Dr. Chuong, this may be a promising screening method.
In the report, Dr. Chuong also shared information about the units that are currently conducting expanded NIPT testing in Vietnam today. Accordingly, in addition to detecting common syndromes, GENTIS also offers extensive NIPT test kits, which can screen for 86 micro-deletion/duplication mutations and NIPT tests in cases of multiple pregnancies.
 Nguyen Canh Chuong, MSc. MD. (Director of Hanoi Hospital of Obstetrics and Gynecology) presented the report: "Expanded NIPT: From a clinical perspective"
Nguyen Canh Chuong, MSc. MD. (Director of Hanoi Hospital of Obstetrics and Gynecology) presented the report: "Expanded NIPT: From a clinical perspective"
In addition, GENTIS was also honored to provide information and data on FSH receptor polymorphic testing for the report of Assoc.Prof. Le Minh Tam PhD.MD. (Director of the Center for Reproductive Endocrinology and Infertility, Hue University of Medicine and Pharmacy Hospital) with the topic: "The role of genetics in low responsiveness of ovarian stimulation".
According to Associate Professor Tam, the identification and classification of patients in the group of poor or good ovarian response is the key to choosing the correct treatment strategy. Along with other factors affecting the ovarian stimulation response, Assoc. Prof. Tam believes that FSH receptor polymorphism is a useful tool for predicting and personalizing ovarian stimulation treatment, helping to achieve the right number of ovums for IVF in fewer stimulation cycles.
 Assoc. Prof. Le Minh Tam, PhD.MD. (Director of the Center for Reproductive Endocrinology and Infertility, Hue University of Medicine and Pharmacy Hospital) presented the report: "The role of genetics in low responsiveness of ovarian stimulation"
Assoc. Prof. Le Minh Tam, PhD.MD. (Director of the Center for Reproductive Endocrinology and Infertility, Hue University of Medicine and Pharmacy Hospital) presented the report: "The role of genetics in low responsiveness of ovarian stimulation"
GENTIS is one of the first units to implement the FSH receptor gene polymorphic test in Vietnam and is continuing to develop clinical studies in infertile women. FSH receptor gene polymorphism promises to be a useful test for doctors, adjuvanting the process of assisted reproductive treatment with good results.
In addition, the conference also had many other scientific reports such as:
- Challenges in current obstetrics and gynecology practice - Prof.Cao Ngoc Thanh PhD. (Vice Chairman of Vietnam Association of Obstetrics and Gynecology)
- Important updated recommendations in obstetrics and gynecology clinical practice - Le Quang Thanh, PhD. (Vice Chairman of the Vietnam Association of Obstetrics and Gynecology)
- Is it necessary to individualize ovarian stimulation in assisted reproduction? - Assoc. Prof. Nguyen Xuan Hoi, PhD.MD. (National Hospital of Obstetrics and Gynecology)
In addition to providing research data to the speakers, GENTIS was also honored to introduce to a large number of delegates participating in the conference the booth to display products with testing solutions from pre-pregnancy, during pregnancy and the newborn stage of the child. This test kit is a tool to support doctors to accompany pregnant mothers, and is the golden key to a perfect start for their children. In particular, GENTIS also sent doctors a lot of gratitude gifts.
 Product display booth of GENTIS attracted great attention from distinguished delegates
Product display booth of GENTIS attracted great attention from distinguished delegates
Through the 10th Open Conference on Obstetrics and Gynecology in the Central-Central Highlands, experts and doctors in the fields of obstetrics and gynecology and reproductive health had the opportunity to exchange experiences in scientific research, diagnosis and treatment. At the same time, they were updated with new clinical knowledge, and discussed and agreed on the development of technical expertise in obstetrics and gynecology. From there, it contributes to the development and improvement of the efficiency of medical health care for the community.
Once again, GENTIS would like to congratulate the Conference on its great success.
The 10th Expanded The Central - Tay Nguyen Obstetrics and Gynecology Conference, organized by the Vietnam Association of Gynecology and Obstetrics (VAGO), has attracted the attention of many experts, doctors, and researchers both domestically and internationally.

This is an opportunity for delegates working in the field of obstetrics and gynecology to enhance their knowledge and expertise through specialized presentations by domestic and international experts. At the same time, participating delegates will update general orientation information and current issues, engaging in discussions within the specialty.
Participating in this event, GENTIS Company is honored to bring many exciting programs, including:
- Exhibition booth of testing services at the conference
- Appreciation gifts for esteemed doctors
We sincerely invite all doctors to follow the conference agenda:




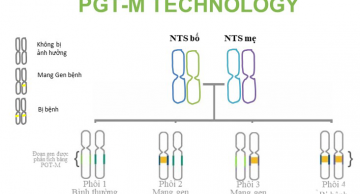
Meaning of the PGT-M test
PGT-M pre-embryo transfer genetic screening test helps couples choose gene-free/disease-free embryos to transfer into the mother's uterus to eliminate genetic mutations that cause disease in the next generation.

The PGT-M test will need to use the embryo sample and the reference sample as follows:
Sample of biopsied embryo (Day 3-5) or WGA product
Reference Sample
- Mandatory reference sample: Sample of Embryo's biological parents: 2-3ml of whole blood in an EDTA anticoagulant tube (with genetic test result information).
- Reference sample 3: Sample of the couple's existing child(s) who want to do PGT-M: 2-3ml of whole blood contained in an EDTA anticoagulant tube.
- Additional reference samples: in some cases, additional samples from the Embryo's grandparents may be requested: 2-3ml of whole blood contained in the EDTA anticoagulant tube.
Note: At a minimum, there must be a parent's reference sample.
The doctor will indicate embryo screening when it is known that the parent carries a mutation in one or more genes that cause the genetic disease. To determine whether you are a carrier of the abnormal gene or not, you can perform tests such as 13 hidden diseases combo, UltraGen at GENTIS to detect mutated genes.
PGT-M Test Procedure at GENTIS

Testing technology: MiSeq next-generation genome sequencing system.
+ Directly identify mutations on embryos (for point/indel mutations of less than 5 nucleotides).
+ Associated genetic analysis using SNPs located close to 2 sides of the mutation to be investigated.
+ Result turnaround time: Excluding public holidays
+ 12 days for 3 diseases: Myeloid atrophy, Duchenne muscle atrophy, Hemophilia, Thalassemia.
+ 30 days for diseases: G6PD enzyme deficiency, Phenylketonuria, Citrin deficiency, Wilson, Pompe, Cystic fibrosis, Fabry, Galactose metabolism disorder TYPE 1, Congenital hearing impairment, Adrenoleukodystrophy.
+ For other diseases, the result turnaround time depends on the types of gene mutations of the parents, for rare mutations, the time may be longer.
List of monogenic diseases performing PGT-M testing at GENTIS
|
No. |
DISEASE |
GENE NAME |
DISEASE INFORMATION |
|
1 |
Thalassemia |
HBA1, HBA2, HBB |
Thalassemia is a blood genetic disease that is associated with a gene mutation that regulates the production of hemoglobin. The main manifestations are anemia and hemochromatosis, and many patients with thalassemia (congenital hemolysis) need to receive blood transfusions and take iron chelators for life. |
|
2 |
Spinal muscular atrophy (SMA) |
SMN1 |
Spinal muscular atrophy (SMA) is a genetic disease that gradually destroys motor neurons – nerve cells in the brainstem and spinal cord that control essential musculoskeletal activity such as speaking, walking, breathing, and swallowing, leading to muscle weakness and atrophy. |
|
3 |
Duchenne muscular atrophy |
DMD |
Duchenne muscular atrophy is a disease that makes muscles weaker and less flexible over time. The muscles in the legs are usually one of the first and most visible affected sites. Children may be able to walk later, fall more easily, and have trouble climbing stairs or getting up. |
|
4 |
Hemophilia A |
F8 |
Hemophilia is a genetic bleeding disease associated with the sexual X chromosome caused by a decrease in factor VIII (hemophilia A) or factor IX (Hemophilia B) leading to thromboplastin dysplasia that delays blood clotting. People with Hemophilia, who are deficient in blood clotting factor, or have low levels of the factor compared to normal people, which makes it difficult for blood clots to form. |
|
5 |
Hemophilia B |
F9 |
|
|
6 |
Congenital adrenal hyperplasia (CAH) |
CYP21A2 |
Congenital adrenal hyperplasia (CAH) is one of the hereditary endocrine diseases, which occurs due to disorders of adrenal hormone synthesis. Causes acute adrenal insufficiency and affects the development of the genital organs. |
|
7 |
G6PD deficiency |
G6PD |
As the most common enzymatic disease on X chromosomes, boys are more susceptible to it than girls. Red blood cells will be destroyed, causing anemia due to hemolysis, mental and motor retardation, jaundice, and dark urine. |
|
8 |
Phenylketonuria |
PAH |
The disease is characterized by intolerance to the amino acid Phenylalanine in daily meals. If not diagnosed early after birth and treated promptly, the disease can cause irreversible brain damage and mental retardation. |
|
9 |
Citrine deficiency |
SLC25A13 |
The disease causes jaundice and cholestasis in infants. Children under 1 year old have a history of low weight and growth restrictions. Beyond 1 year old, children have symptoms such as hypoglycemia, pancreatitis, severe fatigue, loss of appetite, and decreased quality of life. Heavy weight usually begins suddenly in adulthood. Neurological symptoms appear. |
|
10 |
Wilson's disease |
ATP7B |
It is a type of genetic disorder due to genetic abnormalities that causes the body to not eliminate residual copper, leading to the accumulation of copper in body tissues (liver, brain, eyes and other organs) and causing toxicity to the patient, even life-threatening |
|
11 |
Pompe’s disease |
GAA |
Pompe's disease (PD) is a genetic metabolic disorder caused by a deficiency of acid α-glucosidase (GAA), which leads to the accumulation of glycogen in lysosomes, mainly in the skeletal muscle and heart muscle as well as the nervous system. Symptoms that appear immediately after the child is born include: weak muscle tone, eating difficulty, slow weight gain, heart defects, shortness of breath, swelling of the tongue, enlarged liver, weakened liver function, hearing loss,... |
|
12 |
Fabry's disease |
GLA |
Fabry's disease is a type of inherited metabolic disorder, characterized by a deficiency of alpha-Galactosidase enzyme that causes a number of pathological conditions such as keratotic angiomas, corneal opacity, limb paresthesia, renal failure, heart failure, etc. |
|
13 |
Metabolic disorder of galactose type 1 |
GALT |
This is a disease that causes disorders in the conversion of galactose into glucose, causing children to not be able to convert this sugar into energy to be used but accumulate in the blood. Early manifestations in the first few weeks after birth such as poor feeding or skipping breastfeeding, diarrhea, vomiting, coma, physical examination showing jaundice, subcutaneous hemorrhage, hepatomegaly, cataracts. |
|
14 |
Congenital hearing loss |
GJB2 |
60% of children are born with bilateral birth defects due to genetics And abnormalities of the GJB2 gene (recessive gene on autosomal chromosomes) are the most common cause of congenital hearing loss in children. Screening is no later than 1 month old for early detection and intervention, limiting the impact on children's language development. |
|
15 |
Metachromatic leukodystrophy (MLD) |
ARSA |
Metachromatic leukodystrophy (MLD) is one of the diseases related to lipid storage, which causes a toxic accumulation of abnormal fats, which interfere with normal fats and proteins in the myelin shell. From 1-2 years of age, decreased muscle tone, behavioral decline, later paralysis, visual atrophy. Precocious puberty; from 5 to 10 years old, paralysis, epilepsy, death after 10-20 years. |
|
16 |
Adrenal leukodystrophy (ALD) |
ABCD1 |
Adrenal leukodystrophy is a genetic disorder that occurs mainly in men, affecting the nervous system and adrenal glands. This is the most common hereditary disorder (peroxisome), caused by a gene mutation on chromosome Xq28, which has now isolated more than 200 mutations. |
|
17 |
Ornithine transcarbamylase deficiency (OTC) |
OTC |
Ornithine transcarbamylase (OTC) deficiency is a genetic disorder that causes ammonia to build up in the blood. Infants with OTC deficiency may lack energy (apathy) or do not want to eat, and have poorly controlled breathing rates or body temperature. Complications due to ornithine transcarbamylase deficiency may include developmental delays and intellectual disability. Progressive liver damage can also occur. |
|
18 |
Congenital hypothyroidism |
SLC26A4 |
It is a thyroid hormone deficiency disease caused by thyroid development problems or thyroid hormone biosynthesis disorders. |
|
19 |
Smith-Lemli-Opitz syndrome |
DHCR7 |
Smith-Lemli-Opitz syndrome is a disease that disrupts the biosynthesis of cholesterol (reduced). Manifestations of intellectual retardation (100%); microcephaly (90%), cleft palate, small palate, heart defects; underdeveloped external genital organs in men; musculoskeletal deformities. |
|
20 |
HLA conformity |
Determine whether the embryo is suitable for HLA for the sick person so that after the baby is born, there will be a plan to store umbilical cord blood for stem cell transplantation. |
|
|
21 |
Cystic fibrosis (CF) |
CFTR |
Cystic fibroids, also known as cystic fibroids, are genetic disorders that cause the body to produce excessive sweat and mucus. The disease affects the functioning of the lungs, digestive system and genital organs. |
|
22 |
Cartilaginous dysplasia (Achondroplasia) |
FGFR3 |
Achondroplasia is a rare group of inherited bone disorders. This is the most common form that has ever been called dwarfism, in which a child's arms and legs are short compared to their body length. The average height of adult males and females with achondroplasia is about 132cm and about 124cm, respectively. |
|
23 |
Vitreous bone disease |
COL1A1, COL1A2 |
Vitreous bone is a phenomenon of brittle, fragile bones, and incomplete bone formation. The main reason for this condition is a disruption in the genetic process that makes bones fragile even under the influence of a small impact or injury. |
|
24 |
Autosomal dominant polycystic kidney disease (ADPKD) |
PKD1, PKD2 |
Hereditary polycystic kidney disease is a genetic disorder in which clusters of cysts develop inside the kidneys, causing the kidneys to gradually increase in size and decline in function over time. |
|
25 |
Familial hypercholesterolemia (FH) |
LDLR |
People with familial hypercholesterolemia are basically born with high levels of LDL cholesterol. People's cholesterol levels tend to increase with age, however, people with familial hypercholesterolemia have very high levels of baseline LDL cholesterol and rise faster over time. |
|
26 |
Alport Syndrome |
COL4A5 |
Alport syndrome (hereditary nephritis) is a disease that damages the small blood vessels in the kidneys by attacking the renal platelets (the smallest filtration unit in the kidneys), leading to kidney disease and eventually kidney failure. |
|
27 |
Brugada syndrome |
SCN5A |
Brugada syndrome is one of the most common causes of sudden death with causes related to cardiovascular diseases. The disease has the potential to cause life-threatening arrhythmias. People with this syndrome are at high risk of experiencing arrhythmias that originate from the ventricles located in the lower part of the heart. |
|
28 |
Ichthyosis vulgaris |
FLG |
Ichthyosis is a condition in which the skin is damaged mainly due to genetics. Dead skin cells accumulate into patches of skin, thick and dry pieces like fish scales on the surface of the skin. The disease usually appears between the ages of 0 and 7 years, and there are even cases where the disease appears immediately after childbirth. |
|
29 |
Marfan’s syndrome |
FBN1 |
Marfan’s syndrome in people with long limbs and long fingers is a genetic disorder that affects connective tissue. The most obvious signs of this disorder include height, thinness, abnormally long limbs, disproportionately long fingers and toes, protruding or concave sternum, curved spine, loose joints, large and flat feet, severe myopia. |
|
30 |
Hemophagocytic Lymphohistiocytosis (HLH) |
PRF1 |
Hemophagocytic syndrome is a rare blood disease with a mortality rate of 15-60%, a common disease in children under 10 years old, for the primary form usually appears in children under 1 year old while the secondary form does not develop until about 6 years old. This is a syndrome in which histiocytic hyperactivity increases leading to erythrocytes, platelets, and white blood cells to be phagocytized. |
PGT - The Golden Key to Finding Children for Families
The invention of in vitro fertilization (IVF) has helped millions of infertile couples realize their dream of having children after years of waiting. However, couples needing IVF are often older or have issues that reduce the quality of their eggs/sperm. Therefore, embryo transfer often fails or, if successful, may carry risks of having children with birth defects.

Preimplantation genetic testing (PGT) has become an important solution to help couples undergoing IVF achieve successful embryo transfer and give birth to healthy babies.
PGT has become the "golden key" in families' journey to find children, helping to:
- Increase pregnancy rates per embryo transfer
- Reduce miscarriage rates
- Reduce the risk of multiple pregnancies
- Increase the chance of having healthy children
- Reduce the time and resources needed
Given the immense significance of PGT testing, couples should consider getting tested if recommended by their doctor to increase their chances of successful pregnancy and giving birth to a healthy baby.
History of PGT Testing Development at GENTIS
GENTIS Testing Center is proud to be a pioneer in PGT testing in Vietnam, helping countless families turn their dream of having children into reality. Let's take a look at GENTIS's impressive milestones in its 10 years of PGT testing development.
.jpg)
2013: The first NGS Illumina system for PGS (now PGT) testing was imported to GENTIS.
2014: PGT testing was assessed for its value in use at some of the first IVF centers in Vietnam.
2015:PGT testing was officially implemented in Vietnam.
2016-2018: PGT testing volume increased significantly, with more and more IVF centers referring patients for PGT testing.
2019-2022: PGT became a familiar test for IVF centers nationwide.
2023: GENTIS became the first organization in Vietnam to achieve ISO 15189:2012 certification for PGT-A testing services, a testament to the tireless efforts of all GENTIS Testing Center staff.

Up to now, GENTIS has performed testing for approximately 30 IVF centers in Vietnam, with a volume of over 30,000 embryos per year.
In particular, GENTIS has published numerous scientific research papers on PGT in reputable international journals and presented reports at international conferences, including:
- The research paper "Development and clinical application of a preimplantation genetic testing for monogenic disease (PGT-M) for beta thalassemia in Vietnam" was published in the Journal of Assisted Reproduction and Genetics by the American Society for Reproductive Medicine (ASRM).
- A report on the topic "PGT-M for rare diseases in Vietnam" at the ASPIRE 2021 conference.
- A report on "One case of preimplantation genetic testing for Marfan’s syndrome in Vietnam" at the 19th International Preimplantation Genetic Diagnosis Society (PGDIS) conference.
- A report on "A comprehensive pre-implantation genetic test for alpha and beta thalassemia disease" at the 19th International Preimplantation Genetic Diagnosis Society (PGDIS) conference.
With a 10-year journey of implementing and developing PGT testing, GENTIS has made a significant contribution to helping couples select genetically high-quality embryos, increasing the chances of successful pregnancy when undergoing IVF, ensuring that children born are healthy and free from the screened genetic syndromes.
[content_more] => [meta_title] => GENTIS's History of PGT Testing Development [meta_description] => GENTIS is a pioneer in PGT testing in Vietnam. Since 2013, GENTIS has established infrastructure and medical equipment to perform PGT tests. [meta_keyword] => Gentis,PGTTESTING,PGT [thumbnail_alt] => [post_id] => 1157 [category_id] => 4 ) )GENTIS sponsored and presented at the assisted reproductive technology (ART) symposium titled "A Christmas Gift - A Happy Beginning”.
GENTIS partnered with the program “Gifts gleaming - Christmas cheer” at Thanh Nhan Hospital
GENTIS sponsored and reported at the HASAM 2023 Annual Scientific Conference
GENTIS - Gold Sponsor of the HASAM 2023 Annual Scientific Conference
GENTIS co-sponsored the 10th Open Central region and Central Highlands Obstetrics and Gynecology Conference
GENTIS Partners with The 10th Expanded The Central - Tay Nguyen Obstetrics and Gynecology Conference
Monogenic diseases that can be detected with the PGT-M test at GENTIS
GENTIS's History of PGT Testing Development
Please fill in the information below to receive our supports and consultations!
Please fill in the information below to receive our supports and consultations!